+++++++++++++++++++++ The sternocleidomastoid muscle (SCM) divides each side of the neck into two major triangles, anterior and posterior. The anterior triangle is delineated by the anterior border of the SCM laterally, the midline medially, and the lower border of the mandible superiorly. The borders of the posterior triangles are the posterior border of the SCM anteriorly, the clavicle inferiorly, and the anterior border of the trapezius muscle posteriorly.1
In the midline, from above downward, the following landmarks are noted:
|

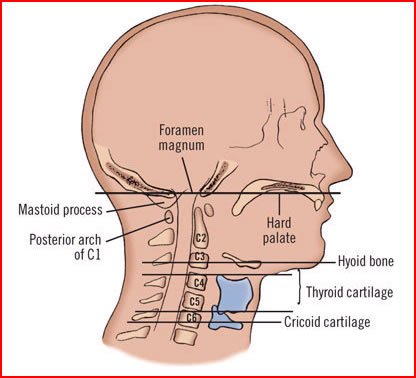 The third cervical vertebra is at the level of the hyoid bone; the fourth and fifth cervical vertebrae are at the level of the thyroid cartilage.
The third cervical vertebra is at the level of the hyoid bone; the fourth and fifth cervical vertebrae are at the level of the thyroid cartilage.

 Seventh cervical vertebra.
Seventh cervical vertebra.
 Diagrammatic cross section through the neck below the hyoid bone showing the layers of the deep cervical fascia and the structures that they envelop.
Diagrammatic cross section through the neck below the hyoid bone showing the layers of the deep cervical fascia and the structures that they envelop.
References
1. ttp://www.med.umich.edu/lrc/coursepages/M1/anatomy/html/surface/index.html#headneck
It is convenient to use the level system to describe the location of lymph node disease in the neck. Level I contains the submental and submandibular nodes. Levels II through IV contain lymph nodes along the jugular vein (upper, middle and lower). Level V contains the lymph nodes located along the lower half of the spinal accessory nerve and the transverse cervical artery, posterior to the SCM. The supraclavicular nodes are included in the posterior triangle group. The pre- and paratracheal nodes, precricoid (Delphian) node, and perithyroidal nodes are found within level VI. Lymph nodes are located throughout the head and neck region and are the most common sites of neck masses.1
Reference
1. http://www.redorbit.com/news/health/98241/evaluation_of_the_neck_mass/#XjFqu7aWpmmRmg1x.99
Laterally, it is bounded by the anterior belly of the digastric muscle, and the mylohyoid muscle forms the floor. The body of the hyoid bone lies opposite the third cervical vertebra. The area between the hyoid bone and the thyroid cartilage is the thyrohyoid membrane, while the notched upper border of the thyroid cartilage is at the level of the fourth cervical vertebra. The cricothyroid ligament or membrane occupies the space between the thyroid cartilage and the cricoid cartilage, which lies at the level of the sixth cervical vertebra and the junction of the pharynx with the esophagus. The interval between the cricoid cartilage and the first tracheal ring is filled by the cricotracheal ligament. Moving inferiorly, the isthmus of the thyroid gland is at the level of the second, third, and fourth tracheal rings. The suprasternal notch can be palpated between the clavicular heads and lies opposite the lower border of the body of the second thoracic vertebra. The sternocleidomastoid muscles, which divide the sides of the neck into anterior and posterior triangles, can be palpated from sternum and clavicle to the mastoid process. The borders of the posterior triangle are the body of the mandible, the sternocleidomastoid muscle anteriorly, and the border of the trapezius muscle posteriorly, along with the clavicle inferiorly.
Posteriorly, the structures of the neck that can be palpated in the midline are the external occipital protuberance, the nuchal groove, and the spinous process of the seventh cervical vertebra (cervical spines 1–6 are covered by the ligamentum nuchae).
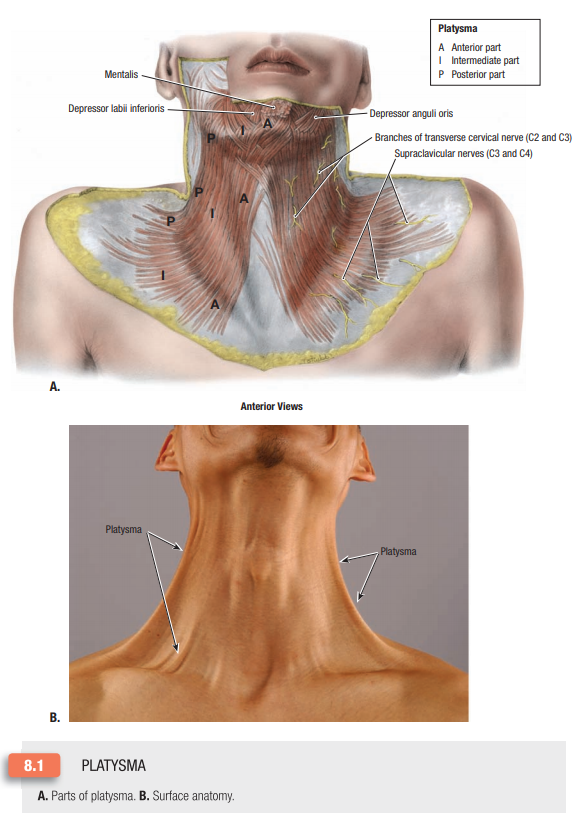
The platysma, a thin muscular sheet, is enclosed by the superficial fascia. Its origin is from the deep fascia that covers the upper part of the pectoralis major and deltoid muscles, and it inserts into the lower margin of the body of the mandible. It is the anatomic landmark that is often cited when determining whether a penetrating wound of the neck is superficial or deep. The potential for injury to a vital structure exists when this structure is penetrated.
Beneath the superficial sternocleidomastoid, strap, and trapezius muscles that envelop much of the neck, there are eight body systems that lie within or pass through the neck. Included among these are the following: (1) skeletal system (seventh cervical vertebra, hyoid bone); (2) nervous system (spinal cord and the glossopharyngeal [IX], vagus [X], spinal accessory [XI], and hypoglossal [XII] cranial nerves); (3) respiratory system (oropharynx, larynx, cervical trachea); (4) gastrointestinal system (oropharynx, cervical esophagus); (5) vascular system (common, internal, and external carotid arteries, vertebral arteries, internal and external jugular veins); (6) lymphatic system (thoracic duct); (7) endocrine system (thyroid and parathyroid glands); and (8) immune system (cervical extensions of the thymus).
|
The muscle attaches to the superior aspect of the manubrium sternum by a tendinous head and from the medial third of the clavicle by a muscular head. It passes superiorly in a lateral, and then posterior, direction. Its superior attachment is to the mastoid process, and the lateral end of the superior nuchal line. Unilateral contraction of the muscle approximates the ear to the ipsilateral shoulder, while rotating the chin to the contralateral side. Bilateral contraction of the muscle can result in either flexion or extension of the head. If the head is slightly flexed, bilateral contraction will result in increased flexion. If the head is slightly extended, bilateral contraction will result in increased extension. The pulsation of the carotid artery is palpable, anterior to the edge of the muscle.
The anterior tuberosity of the transverse process of the sixth cervical vertebra is located at the medial border of the sternocleidomastoid and at the level of the cricoid cartilage. Pressure at this point will compress the common carotid artery.
|
 The third cervical vertebra is at the level of the hyoid bone; the fourth and fifth cervical vertebrae are at the level of the thyroid cartilage.
The third cervical vertebra is at the level of the hyoid bone; the fourth and fifth cervical vertebrae are at the level of the thyroid cartilage.

 Seventh cervical vertebra.
Seventh cervical vertebra.
 Diagrammatic cross section through the neck below the hyoid bone showing the layers of the deep cervical fascia and the structures that they envelop.
Diagrammatic cross section through the neck below the hyoid bone showing the layers of the deep cervical fascia and the structures that they envelop.
References
1. ttp://www.med.umich.edu/lrc/coursepages/M1/anatomy/html/surface/index.html#headneck
__________________________________________________________
-
Trapezius muscle that has a very broad origin from the medial portion of the superior nuchal line, external occipital protuberance, ligamentum nuchae, spinous processes, and the supraspinous ligaments of the thoracic vertebrae. The muscle fibers converge and insert on the lateral third of the clavicle and the acromion process of the scapula. Because of the extensive origin of the muscle, differential contraction will create different movements. Contraction of the upper fibers will cause elevation of the scapula. Depression of the scapula is created by contraction of the inferior fibers. The middle fibers will cause the medial edge of the scapula to approach the midline. The external branch of the accessory nerve provides innervation to the trapezius and sternocleidomastoid muscles. Branches from the second and third cervical nerves provide added innervation.
-
Mastoid process.
-
Ramus of mandible.
-
Hyoid bone, palpable in the midline of the neck when the mandible is slightly depressed. It is located at the level of the third cervical vertebra. The greater horn of the hyoid bone can be traced to its lateral termination. This is the approximate level of origin of the lingual branch of the external carotid artery. The superior thyroid branch arises just inferior to this point, and the facial branch begins just superior to the same palpable landmark.
-
Fused laminae of the thyroid cartilage. The upper edge of this palpable structure is situated at the level of the fourth cervical vertebra. It represents the site of bifurcation of the common carotid artery.
-
Arch of the cricoid cartilage, palpable below the inferior end of the thyroid laminae. A small defect separates them. The cricoid cartilage represents an “anatomical bonanza” because it is a landmark for many anatomical occurrences. It may be referred to as the “cricoid plane.”
-
The larynx ends, and the trachea begins.
-
The pharynx ends, and the esophagus begins.
-
The cricoid cartilage is at the level of the sixth cervical vertebra.
-
The intermediate tendon of the omohyoid muscle is found anterior to the carotid sheath.
-
The inferior thyroid artery passes posterior to the carotid sheath on its way to the lateral lobe of the thyroid gland.
-
The middle cervical sympathetic ganglion lies on the transverse mass of the sixth cervical vertebra.
-
The recurrent laryngeal nerve enters the larynx.
-
The ansa cervicalis is found anterior to the carotid sheath.
-
The vertebral artery enters a foramen in the transverse mass of the sixth cervical vertebra. This occurs at the apex of a muscular triangle formed by the anterior scalene and longus coli muscles. The base of the triangle is the first portion of the subclavian artery.
-
TThe superior pair of parathyroid glands is often found at this level.
-
-
Upper tracheal rings that are palpable between the cricoid cartilage and the superior edge of the manubrium sternum.
-
Superior edge of the manubrium of the sternum. It is at the level of the second thoracic vertebra.
from the atlas down to the upper sacral segment. It is attached to the intervertebral disc and that portion of the vertebral body lying just superior and inferior to the disc. The nuchal ligament covers the spinous processes of all the cervical vertebrae.
traveling with the hypoglossal nerve, provide motor innervation to the thyrohyoid and geniohyoid muscles. A branch from C4 descends on the anterior surface of the anterior scalene muscle, within the prevertebral fascia. It is the phrenic nerve and it may receive branches from C3 and C5. It is, at first, seen on the lateral aspect of the anterior scalene muscle, but as it descends it passes obliquely across the anterior surface of the muscle and reaches its medial edge in the root of the neck. It then passes anterior to the subclavian artery and courses medial to the internal mammary artery before entering the thorax. It provides sensory and motor innervation to the respiratory diaphragm (Fig. 2). There are some proprioceptive branches arising from the cervical plexus that pass to the sternocleidomastoid and trapezius muscles.
structures found in this area. Neck structures also contribute to the complexity of the anatomy in this important region. Passing between the clavicle and the first rib are nerves, arteries, and veins of the upper extremity. Narrowing of this costoclavicular canal can cause compression of these neurovascular structures. The thoracic inlet is created by the upper end of the manubrium anteriorly, the first rib and its costal cartilage laterally, and the first thoracic vertebra posteriorly. Structures passing through this area are medial or lateral in position. The esophagus and the trachea are medial as they enter the mediastinum. The thoracic duct lies just to the left of, and posterior to, the esophagus. In the root of the neck, at the level of C7, the duct passes laterally. It courses anterior to the left vertebral and left inferior thyroid arteries and posterior to the carotid sheath. It then travels anterior to the anterior scalene muscle. It is superficial to the prevertebral layer of the deep cervical fascia. The duct then descends anterior to the left subclavian artery and terminates at the lateral edge of the junction between the left internal jugular and the left subclavian veins (see Fig. 5).
thyroid gland. The transverse cervical and the suprascapular arteries are branches of the thyrocervical trunk that run transversely as they head for the lateral aspect of the neck. They cross the anterior scalene muscle and the phrenic nerve, but are superficial to the prevertebral fascia. The transverse cervical artery will divide into an ascending and descending branch when it reaches the margin of the trapezius muscle. The suprascapular artery will dip down below the clavicle after entering the posterior triangle, pass inferiorly, and contribute to the periscapular vasculature.
-
Costoclavicular compression syndrome
-
Cervical rib syndrome
-
Anterior scalene compression syndrome
-
Pectoralis minor syndrome
-
Cervical incisions should be made parallel to the skin lines (lines of Langer) for good cosmesis. The neurovascular structures lie deep to the platysma muscle. The muscle must be carefully repaired for the best cosmetic result.
-
The middle cervical ganglion block: this sympathetic ganglion is found anterior to the transverse mass of the sixth cervical vertebra. At the level of the cricoid cartilage, retract the carotid sheath laterally and inject the medication after the needle strikes the lateral mass of the vertebra.
-
Control of bleeding may be possible if the common carotid artery is compressed against the transverse mass of the sixth cervical vertebra. This is the cricoid plane.
-
Carotid angiography: the common carotid artery is palpable in the carotid triangle. It is partially covered by the sternocleidomastoid muscle. Lateral retraction of the muscle will facilitate insertion of a catheter into the palpable artery.
-
Internal jugular vein catheterization: the internal jugular vein accompanies the common and internal carotid vessels. They all lie within the carotid sheath. The vein is anterolateral to the palpable artery.
-
The right internal jugular and right brachiocephalic veins, along with the superior vena cava, create a straight conduit to the right atrium and the inferior vena cava.
-
The subclavian vessels can be approached while passing through the costoclavicular space. The artery is palpable and the vein is situated anterior and medial to the artery. The vein is the most medial structure passing through the costoclavicular interval. A supraclavicular, or infraclavicular, technique can be used for catheterization.
-
The brachial plexus block approaches the nerves as they pass through the costoclavicular space. The subclavian artery is anterior to the branches of the plexus.
-
In cricothyroidotomy, the interior of the larynx is entered through the cricothyroid interval. The cricothyroid artery, a branch of the superior thyroid, pierces the cricothyroid ligament near the middle of the interval between the cricoid and the thyroid cartilages. A transverse incision, made close to the upper border of the cricoid arch, will avoid injury to this artery. The vocal ligaments are spared because they are superior to the point of entry.
-
For drainage of the retropharyngeal space, an incision is made at the level of the cricoid cartilage. The sternocleidomastoid muscle and carotid sheath are retracted posteriorly, and the lateral lobe of the thyroid gland is retracted anteriorly.
-
Using the external jugular vein as a conduit for central venous access, the external jugular vein is readily accessible because of its superficial position. It empties into the subclavian vein in the posterior triangle, but it may be difficult to negotiate the angle at the termination when attempting to introduce a device into the central portion of the circulatory system. Direct approach to the larger veins, right internal jugular or right subclavian, would eliminate this technical problem.

|
Fig. 6. Boundaries of the triangles of the neck (see also Fig. 14).
 |
piercing the thyrohyoid membrane. It provides sensory innervation to the interior of the larynx above the vocal ligaments. The external branch passes inferiorly, in contact with the inferior constrictor, and gives some branches to this muscle. It also provides motor innervation to the cricothyroid, one of the intrinsic muscles of the larynx. This nerve, for a portion of its course just superior to the thyroid gland, is very close to the medial side of the superior thyroid vascular bundle. It should be located and swept medially in order to avoid its injury when ligating and dividing these blood vessels. In the superior part of this triangle, the spinal accessory nerve is seen as it passes inferolaterally, deep to the sternocleidomastoid muscle, and enters the posterior triangle.
and posterior auricular arteries. The occipital branch runs along the inferior edge of the posterior belly of the digastric muscle. The posterior auricular branch follows a similar course on the superior aspect of this important muscle. The external carotid artery continues superiorly to the parotid region. At the neck of the condylar process of the mandible, the end branches arise. They are the superficial temporal and internal maxillary arteries.
the deep cervical plexus (C1, C2, and C3) by way of the ansa cervicalis. The nerves enter the inferior portion of the muscle. A branch of C1, which travels with the hypoglossal nerve, innervates the thyrohyoid muscle.
-
Transection of strap muscles should be done closer to the superior end to preserve nervous innervation, which enters the muscle near its inferior end.
-
Proper entrance into the cleavage plane between the sternothyroid muscle and the thyroid gland provides excellent exposure of, and facilitates surgical approach to, the gland.
sternocleidomastoid. The C5 and C6 roots combine to create the upper trunk, C7 becomes the middle trunk, and C8 and T1 create the lower trunk. The trunks are seen in the posterior triangle. There are branches arising from these roots and trunks that are seen in the posterior triangle. The dorsoscapular nerve (C5) pierces the middle scalene muscle and passes laterally toward the rhomboid and levator scapula muscles, which it innervates. The long thoracic nerve (C5, C6, and C7) courses inferiorly, passes deep to the other portions of the brachial plexus, and then passes over the first rib to reach the superficial surface of the serratus ventralis, where it innervates. Arising from the upper trunk of the plexus is the suprascapular nerve, which is seen just above the upper trunk, passes across the posterior triangle to the scapula, and innervates the supraspinatus and infraspinatus muscles. The subclavius nerve is also seen in the posterior triangle. It arises from the upper trunk, passes inferiorly, and crosses the main portion of the brachial plexus superficially. It innervates the subclavius muscle.
travel with this cranial nerve. These nerves, and the spinal accessory nerve, are the only motor branches that are superficial to the prevertebral layer of the deep cervical fascia in the posterior triangle.
plexus, and the spinal accessory nerve, are quite close to each other as they first appear in the posterior triangle at the edge of the sternocleidomastoid muscle. If one divides the posterior edge of this muscle into thirds, at the junction of the middle and superior third is the site where all these nerves can be found gathered in a small localized area. This is referred to as the nerve point. They will then diverge as they head toward their specific destinations. As the nerves pass through the posterior triangle, it will be seen that the spinal accessory nerve is the most superior of all the nerves that are in the triangle. Therefore, incisions that are made superior to the spinal accessory nerve are not likely to encounter any important nerves. This area has been referred to as the carefree area; whereas, an incision made below this nerve can injure major structures and is called the careful area.
-
Superficial cervical plexus nerve block. The nerve point is located and the local anesthetic is injected in that region of the posterior edge of the sternocleidomastoid muscle. It can provide adequate anesthesia to the anterior triangle if bilateral nerve point injection is performed.
-
Catheterization of the subclavian artery or vein. The third portion of the artery is palpable as it passes between the midportion of the clavicle and the first rib. The accompanying vein is anteroinferior to the artery and is the most medial of the neurovascular structures that pass through the costoclavicular space.
-
Dissection can be performed safely in the posterior triangle in the area superior to the spinal accessory nerve (XI).
-
There are one or two motor branches for the trapezius muscle that originate from the deep cervical plexus. They run with, but are slightly inferior to, the spinal accessory nerve in the posterior triangle. In this area, these cervical nerves and the spinal accessory nerve are the only motor nerves that lie external to the prevertebral layer of the deep cervical fascia.
-
When veins pass through layers of fascia, the wall of the vein is adherent to the margins of the opening in the tissue being breached. If a vein is transected at the level of fascia penetration, bleeding may be prolonged because the attachments to the vessel wall may prevent it from going into spasm. Spasm of the cut end of a blood vessel assists in achieving hemostasis.
esophagus, cricothyroid and inferior constrictor muscles, external branch of the superior laryngeal, and the recurrent laryngeal nerves. The carotid sheath and inferior thyroid artery are posterior. The superior thyroid vessels and the external laryngeal branch of the superior laryngeal nerve approach the lobe from above. The sternohyoid, omohyoid, and sternothyroid muscles are anterior relations. The left lateral lobe is related to the thoracic duct as it travels superiorly, just to the left of the esophagus. It maintains this position until C7, where it arches laterally.
that cross the midline by way of the isthmus. The posterior branch of the superior thyroid artery communicates with branches of the inferior thyroid artery. The venous drainage is via the superior thyroid vein into the internal jugular or common facial vein, the short middle thyroid vein into the internal jugular vein, and the inferior thyroid veins into the brachiocephalic vein.
-
A parathyroid gland may resemble a small lymph node, but the glandular tissue is softer when palpated, compared with the firmer feel of the node.
-
Superior enlargement of the thyroid lobe is prevented by the insertion of the sternothyroid muscle into the oblique line of the thyroid cartilage. Lateral expansion can occur.
-
Occasionally, there may be extralaryngeal branching of the recurrent nerve, resulting in loss of a single main trunk. This will usually occur superior to the inferior thyroid artery. Therefore, it is better to look for the main trunk of the nerve inferior to the artery.
-
The inferior thyroid artery will usually divide into two or three branches before entering the parenchyma of the thyroid gland. The recurrent nerve usually passes between these branches.
-
If the inferior thyroid artery is divided laterally, just after passing posterior to the carotid sheath, nerve injury is unlikely.
-
Anteromedial retraction of the lateral lobe of the thyroid gland will displace the recurrent laryngeal nerve from its expected position in the tracheoesophageal groove, toward the posterolateral aspect of the trachea.
-
There may not be a recurrent laryngeal nerve found in the tracheoesophageal groove if there is a high origin of the nerve. This is referred to as a nonrecurring nerve.
-
A cricothyroidotomy provides access to the infraglottic space. This area of the larynx is below the vocal ligaments.
cartilage in its wall. Passing inferiorly from this elevation is the salpingopharyngeal fold, created by the salpingopharyngeus muscle. Posterior to the bulge and the fold is the pharyngeal recess. On the posterior wall, there may be collections of lymphatic tissue referred to as pharyngeal tonsils, or adenoids. An anterior wall is created by the nasal cavity.
-
Stylohyoid ligament is found between the tip of the styloid process of the skull and the lesser horn of the hyoid bone (Fig. 25). It supports the hyoid, and through theP.289
thyrohyoid membrane is also responsible for suspension of the larynx. -
Pharyngeal raphe is a fibrous seam, which represents the posterior site of attachment for the left and right constrictor muscles. It is attached superiorly to the pharyngeal tubercle found on the basal portion of the occipital bone, 1/2 in. anterior to the foramen magnum. Inferiorly, it merges with the esophageal wall.
-
Pterygomandibular raphe is a fibrous structure between the pterygoid hamulus and the mandible. It provides attachment for the superior constrictor and the buccinator muscles.
pharyngeal plexus. The superior laryngeal nerve arises from the vagus at the base of the skull. It creates the external laryngeal nerve, which innervates the lower portion of the inferior constrictor, and the cricothyroid muscle of the larynx.
muscles. The stylopharyngeus muscle receives motor innervation from the glossopharyngeal nerve. The superior laryngeal nerve arises from the vagus at the base of the skull. It creates the external laryngeal nerve that innervates the lower portion of the inferior constrictor and the cricothyroid muscle of the larynx. The remainder of the muscular wall receives motor innervation from the pharyngeal plexus. Sensory innervation is provided by the glossopharyngeal nerve via the pharyngeal plexus.
interarytenoid fold. The mucosa covering the superior edge of the quadrangular membrane forms the aryepiglottic fold. The space between the aryepiglottic folds is the entrance into the vestibule. It is the laryngeal aditus. The mucosa covering the vestibular ligament creates the vestibular fold, which is the inferior end of the vestibule. The space between the vestibular folds is the rima vestibuli. Below the vestibular folds are the vocal folds. The mucosa covering the vocal ligaments creates the vocal folds. It is very adherent and has a white coloration. The mucosa of this fold is stratified squamous. The remainder of the laryngeal mucosa is pseudostratified ciliated columnar. The space between the vocal folds is the rima glottidis. It is found 1/4 in. below the rima vestibuli and is easily visualized by endoscopic examination through the wider rima vestibuli.
directly on the arytenoids, with resultant effect on the vestibular and vocal ligaments. The muscles can be divided into three functional groups. The first provides protection by sphincter-like activities. They are in the aryepiglottic fold. The aryepiglottic muscle passes from the posterior surface of the arytenoids to the lateral aspect of the epiglottis (Fig. 31). The thyroepiglottic muscle extends from the internal aspect of the thyroid lamina to the lateral aspect of the epiglottis. These muscles help close the laryngeal aditus. The second group of muscles tenses, relaxes, or adducts the vocal ligaments. The cricothyroid muscle, found between the arch of the cricoid and the internal aspect of the fused thyroid lamina, causes elevation of the arch of the cricoid and depression of the lamina. This results in tensing of the vocal ligaments. The thyroarytenoid muscle, which is found between the thyroid cartilage anteriorly, and the arytenoids oppose this action posteriorly. It pulls the vocal processes anteriorly and relaxes the vocal ligaments. Fibers from the medial aspect of this muscle attach directly to the vocal ligaments and can cause differential contraction and relaxation of portions of the vocal ligament. These specialized fibers are named the vocalis muscle. The lateral cricoarytenoid muscle, between the posterior portion of the arch of the cricoid and the muscular process of the arytenoids, is the main adductor of the vocal ligaments. The transverse arytenoid is the only unpaired muscle of the larynx; it passes between the arytenoids and causes narrowing of the rima glottidis and the rima vestibuli. The third group of muscles is responsible for widening of the rima glottidis. The posterior cricoarytenoid muscle passes obliquely between the posterior surface of the cricoid lamina and the muscular process of the arytenoid. It widens the rima glottidis by abducting the vocal process of the arytenoid cartilage.
-
Common facial vein is formed by the union of the anterior facial vein with the anterior division of the retromandibular (posterior facial) vein. It passes over the submandibular triangle and the posterior belly of the digastric muscle, and empties into the internal jugular vein in the superior portion of the carotid triangle.
-
External jugular vein is created by the union of the posterior auricular vein with the posterior division of the retromandibular vein. The vein passes inferolaterally, runs obliquely across the superficial aspect of the sternocleidomastoid muscle, pierces the deep cervical fascia in the subclavian division of the posterior triangle, and empties into the subclavian vein. The great auricular nerve (C2, C3) is posterior to this superficial vein in the upper part of the neck.
-
Anterior jugular vein begins in the suprahyoid portion of the neck and descends vertically, close to the midline, down to the clavicle. It then pierces the investing layer of the deep cervical fascia, passes deep to the sternocleidomastoid, and ends in the ipsilateral external jugular vein. It frequently gives a branch in the suprasternal area that crosses the midline and joins with the contralateral anterior jugular vein. This transverse communicating branch is referred to as the jugular venous arch.
-
Vein of Kocher arises in the submandibular area as a branch of the anterior facial vein, descends on the anterior edge of the sternocleidomastoid muscle, and terminates in the jugular venous arch, or the internal jugular vein.
(postauricular), and occipital nodes. It creates a ring of lymph nodes in this area.
-
A vertical group that receives the lymphatic drainage from the superior horizontal components (Fig. 33). There are three pathways possible in this grouping. (a) The posterior cervical group consists of superficial nodes traveling with the external jugular vein and a deep group of nodes that journey with the spinal accessory nerve (XI). They are in the posterior triangle. (b) The jugular group is intermediate in position and is frequently referred to as the deep cervical group. This pathway is the most important. It consists of nodes at several levels, as this vertical channel descends with the internal jugular vein. There is a juguloparotid node located near the angle of the mandible, a jugulodigastric node where the posterior belly of the digastric muscle crosses the internal jugular vein, a jugulocarotid node near the bifurcation of the common carotid artery, and a jugulo-omohyoid node where the omohyoid muscle crosses the internal jugular vein. The jugulodigastric node receives drainage from the tonsil. The jugulo-omohyoid node receives drainage from the tongue. (c) The visceral chain is the most anterior of the vertical pathways and drains all the cervical viscera. The individual components of this nodal chain are parapharyngeal, paralaryngeal, prelaryngeal or Delphian, paratracheal, and pretracheal. The Delphian node is a constant finding and receives lymphatic drainage from the larynx and the thyroid gland.
-
An inferior horizontal group, called supraclavicular nodes, is found in the subclavian triangle. They receive lymphatic flow from the vertical cervical channels and the upper extremity, axilla, and the thoracic wall. They communicate, by way of efferent channels, with internal jugular and subclavian conduits. Some of these supraclavicular nodes lying anterior to the anterior scalene muscle are referred to as scalene nodes. They receive bronchomediastinal channels from the thorax and may be enlarged as a result of spread from an intrathoracic disease process.
-
The thoracic duct receives inflow from all lymphatics below the respiratory diaphragm, the left hemithorax by way of the left bronchomediastinal trunk, the left side of head and neck via the left vertical cervical trunks, and from the leftP.295
upper extremity through the left subclavian trunk. It empties into the venous system on the lateral aspect of the junction between the left internal jugular and the left subclavian veins. The trunks may enter separately into the venous circulation. On the right side, it is unusual for the bronchomediastinal, subclavian, and vertical cervical trunks to combine before entering the venous circulation. They frequently empty, as separate entities, into the vascular compartment.
-
Otorhinolaryngologists were liberated from the destructive surgery, for example, in mastoids and with otitis media, with the advent of effective antibiotics. In addition, pharyngeal neck abscesses from various colds and infections also vanished from the scene with effective antibiotics. Thus, they tried to reinvent themselves in the same area in which they were trained, but in which much of the destructive surgery based on infectious disease was not cared for with antibiotics. In those cases, they turned, as well as others, from destructive surgery to constructive surgery.
-
The rise of oral surgery. Oral surgery emerged as differentiated from dentistry some time in the early 1940s and gradually developed in the 1950s and 1960s. Carcinoma of the tongue, carcinoma of the tonsil, and pharyngeal maxillary cancer to a certain extent. This was also when submandibular cancer became part of the repertoire of the oral surgeon in some geographical areas.
-
General surgeons were held in sway by some leaders who didn't believe in the resection of nodes for thyroid cancer. A papillary carcinoma, of course, has a low mortality, and so it is difficult for some surgeons to believe that general surgeons, especially those taking care of thyroid cancer, should pursue the adenopathy, since mortality is so low. Others believed that carcinoma of the thyroid could be treated with psychiatry. In any event, this tide has turned, and at this point in time, most surgeons dealing with thyroid cancer have gotten much more aggressive at attacking the adenopathy with node dissections.
-
Other specialties began to concentrate on parathyroid surgery, which previously was the field of general surgery and endocrine services. In other chapters of this book, it does appear that the rates of success between ENT surgeons and general surgeons differ. In some of the well-recognized centers for parathyroid surgery, a success rate of 99% is expected. For those in the ENT field, it does appear as if perhaps a 95% or 96% rate of success in “curing” hypoparathyroidism is the norm.
-
The cricoid bone is an anatomic bonanza, as is detailed in this chapter.
-
The superior surfaces of the first rib are flattened, so that neurovascular structures can travel over it without compression. This, of course, is true of thoracic outlet syndrome, in which the vasculature and sometimes the nerves are compressed.
-
The subclavian artery passes over the posterior sulcus of the scalene tubercle. The anterior scalene muscle attaches to the first rib between the subclavian vessels and, therefore, is in a position to compress the subclavian artery, giving rise to the thoracic outlet syndrome.
-
The cervical sympathetic chain has as its apex a “dumbbell-shaped structure, called the cervicothoracic, or stellate, ganglion.” The reason for it being called stellate ganglion is that it is star-like and gives out the multiple branches. The stellate ganglion, when invaded by a tumor at the apex of the lung on one side or the other, gives rise to the Horner's syndrome and is often the first symptom or sign of the presence of that tumor.
-
The brachial plexus is formed by the ventral rami of C5 through T1. These nerve roots will form three trunks—C5 and C6 form the upper trunk, C7 root forms the middle trunk, and C8 and T1 form the lower trunk. These pass between the middle and anterior scalene muscles.
-
The lower trunk of the brachial plexus is draped over the first rib immediately posterior to the subclavian artery.
-
The fascia of the neck: The superficial fascia, which is often is not well developed, forms the platysma, which may or may not be very robust; the cervical branch of the facial nerve enervates the platysma, which contributes to facial expression.
-
The cutaneous branches and the superficial veins are below the muscles of facial expression, which are the platysma.
-
Deep cervical fascia: The superficial or investing layer of the deep cervical fascia splits to surround the trapezius and the sternocleidomastoid muscle and the submandibular and parotid glands.
-
The carotid sheath, which is part of the deep cervical fascia, surrounds the common carotid, the internal jugular, and the vagus nerve. The vagus nerve is between the common carotid and the internal jugular, which is somewhat posterior to the common carotid.
-
When the common carotid artery divides the internal carotid, it immediately goes anterior to the carotid, except at the base of the skull; the vein is anterolateral to the artery.
-
The sympathetic chain is in contact with the posterior sheath.
-
The thoracic duct is to the left of, and posterior to, the esophagus. It enters at the junction of the internal jugular vein and the subclavian vein.
-
The right lymphatic duct, which is the counterpart of the left thoracic duct, is not large as the thoracic duct and consists of several smaller lymphatics. It drains the right upper extremity and the upper right hemithorax.
-
The right recurrent laryngeal nerve loops around the right subclavian. The left recurrent nerve loops the aortic arch on the left. The right recurrent nerve is less well protected, as it comes up lateral to the tracheoesophageal groove, but, to get to the tracheoesophageal groove on the right, it is more superficial and more widely exposed.P.296
-
Sibson's fascia is at the apex of the lung and runs between C7 and the first rib. It is somewhat protective of the apex of the lung.
-
The inferior thyroid artery is superficial to the prevertebral fascia. It courses posterior to the carotid sheath and anterior to the vertebral artery.
-
The last branch given off by the subclavian artery, as it goes from medial to lateral, is the internal mammary, which then travels behind the sternum and attaches to the sternum medial to the ribs.
-
The anatomy of the root-of-the-neck compression syndromes includes the following:
-
Costoclavicular compression syndrome.
-
Cervical-rib compression syndrome.
-
Anterior scalene compression syndrome (thoracic-outlet syndrome).
-
Pectoralis minor syndrome.
The following are the clinical anatomic applications which are practical in the surgery of this area. -
-
Cervical incisions should be made parallel to the skin lines for good cosmesis.
-
Control of bleeding may be possible, if the common carotid artery is compressed against the transverse mass of the sixth cervical vertebra, which is the cricoid plane.
-
The hyoid bone is the central structure of the neck. Most of the structures of the neck—muscular and membranous—attach to the hyoid bone. If one considers the hyoid bone and the attached posterior belly of the digastic muscle, it is possible to divide the anterior triangle into suprahyoid and infrahyoid portions.
-
The vagus nerve is behind and slightly posterior to the carotid and internal jugular vessels.
-
The posterior belly of the digastic muscle is superficial to the neurovascular structures and presses them against the pharyngeal wall. Therefore, owing to this structure, incisions can be made without the risk of injuring the nerves or arteries.
-
The intermediate tendon of the omohyoid between the two bellies is in the cricoid plane with a number of other venous and tendinous structures.
-
The transection of the strap muscles closer to the superior end will preserve the nervous innervation, since the nerve enters the muscle near the inferior end. Most individuals who divide the strap muscles to get at the thyroid do so at the interior end. Personally, I have never been taught that one divides the strap muscles at the superior end because the nerve enters inferiorly, but it is something good to remember, because one of the cosmetic difficulties following thyroid surgery is the denervation of the strap muscles, at times with a bulge in the lower neck.
-
When one enters the cleavage between the sternothyroid muscle and the thyroid gland, this provides excellent exposure of and facilitates surgical approach to the gland, which is avascular.
-
The long thoracic nerve originates from C5, C6, and C7 and courses inferiorly, passing to the other portions of the brachial plexus, and then passing over the first rib to reach the superficial surface of the serratus ventralis, which it innervates.
-
Dissection on the posterior triangle is safe in the area superior to the spinal accessory nerve.
-
A good landmark for the upper thyroid glands is that they are usually at the level of the thyroid cartilage.
-
If there is a high origin of the recurrent laryngeal nerve, it may not be in the tracheoesophageal groove and it is called a nonrecurring nerve. Obviously, if there is a high origin, it is more exposed and not protected by not being in the tracheoesophageal groove.
 A horizontal plane approximately at the junction of the sixth and seventh cervical vertebrae can be associated with the following anatomic entities (Figs.
A horizontal plane approximately at the junction of the sixth and seventh cervical vertebrae can be associated with the following anatomic entities (Figs. 































